Vaccines and ICU: the light at the end of the tunnel
“It was the light at the end of the tunnel”
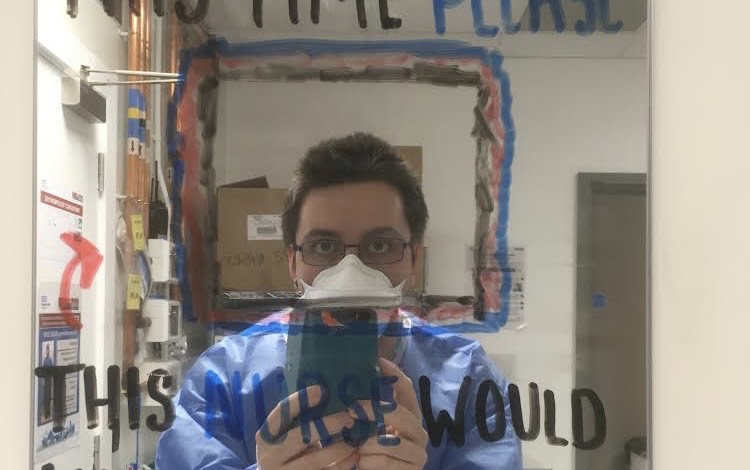
George Huntington, who joined ICU as a junior doctor, describes his experience working on an intensive care unit before and after the rollout of Covid-19 vaccines.
“I joined the adult intensive care unit (ICU) at The Royal London as a senior house office (SHO) at the start of the first wave of the pandemic. I hadn’t worked in this area before and so only had limited experience of looking after these types of patients. But I’d applied because I was interested in training and working in ICU in the future – I like the large teams and the variety and complexity of issues you tend to find on these units.
“Before joining the team, I’d been working in two emergency departments in much smaller hospitals and had seen first-hand the damage coronavirus could do. But it was different working in the ITU. My first shift was working overnight and the unit was full of intubated patients with Covid-19. Capacity was limited – the bay beds were doubled up, squeezing six or eight patients into spaces meant for four. Theatre recovery had been converted into a non-covid ITU and was being staffed mostly by the anaesthetic team. As I joined the fray, I felt useless. All of my experience and confidence drained out of me. I hadn’t prepared for any of this.
Deafened by clanging pots
“The memories of those first nights, beyond the sense that I was out of my depth, were of long shifts in masks, goggles and gowns and meeting my new colleagues through the walkie-talkie system set up to limit waste of PPE – using this system avoided repeated donning and doffing as we entered and left Covid-19 zones. Once you were in, you stayed for as long as you could. At least we as doctors could leave more easily. The nursing teams had to remain at the bedside in their confining PPE for longer periods of time.
“I had seen people pass away before, it is a reality of working in healthcare. But this was different – the sheer numbers of people dying only added to the hopelessness we felt. Patients would come in, work hard to breathe then be intubated. You’d get to know them for a few weeks and they’d slip away. It was hard not to grow hardened to this – we still had to be there for the families who needed comfort, as well as our surviving patients who need our care.
“Though mood was low and people were tired. But there were things which made the situation more bearable. Many organisations kindly donated food, soaps and other products to us. My hands broke out in a rash from where I was washing them so often – at least there was something now to moisturise them with. Once a week I walked through Watney Market to get to work, deafened by clanging pots and rousing applause for the NHS.
A miracle
“When I started working at The Royal London, we were living in lockdown. I only really left my apartment to commute. Outside of work, we avoided talking about the growing pandemic but how could we not? It was everywhere. We obsessed over it, every tiny detail.
“One of those details I remember was there being talk of a future vaccine. The impression was, although it might save us, it would be a long way off – perhaps even years. So, with no end in sight, we knuckled down and focussed on what was in front of us on a day-to-day basis. How wrong we were.
“By the end of 2020, we were slipping into a second wave and London was moving into tier two. At that point, I had given up on following the numbers of new cases, instead trying to focus on gaining non-Covid ITU experience. Over the course two weeks we were swamped with cases again. But this time, something was different. Because at the same time, by some miracle and a lot of hard work and collaboration, the first Covid-19 vaccine was approved and rolled out. I remember wanting to get vaccinated immediately, but because I had coronavirus earlier in the year, I had to delay my course and wait for a slot to became available.
Silence leaves the wards
“ITU filled up again, however this time it was different – the patients didn’t seem as unwell. Though many were still the sickest of the sick, more started to recover. And some didn’t require intubation at all. It was clearly as a result of new treatments like dexamethasone and remdesivir. But there was no doubt that the new vaccine was also having an impact. It stopped people from getting really sick with the virus. It was the light at the end of the tunnel that we all needed.
“I remember many patients were sitting in chairs and bed, able to hold conversations with us. It wasn’t much, but it was an improvement from the ventilator bleeps and silence we’d experienced on the unit and wards during the first wave.
“One by one, we closed the ICU beds that had been opened specifically for Covid-19 patients – there were fewer and fewer patients who needed to be there. We said goodbye to the redeployed staff who’d helped us in the past few months, grateful for their help and at the same time, grateful it wasn’t needed anymore. And gradually, we turned our attention to other areas of work which had to be paused to manage the pandemic.
Playing our parts
“After 18 months on ICU, I left to gain more experience and training in other areas. It’s strange to look back on my time on the unit and say that on the whole I enjoyed it. I know that is in big part thanks to the team there. I’m exceedingly grateful to them for their patience and kindness and for taking the time to help me develop and become a more useful member of the team, even in the midst of the crisis.
“I also look back fondly on the brilliant camaraderie that emerged from the pandemic. There was a spirit of co-operation, kindness and of all of us being in it together. Seeing this effort and cooperation raised my spirits the most, I think. Although it wasn’t the experience I was looking for when I applied for the post, it felt good to be able to contribute to the effort in a small way as opposed to just watching things unfold. And I know that I can cope in these stressful situations, sometimes even thrive in them.
